Patient Selection Criteria
Learn more about Sacroiliac Joint Dysfunction, its treatment algorithm, and more.
What is SI Joint Instability?
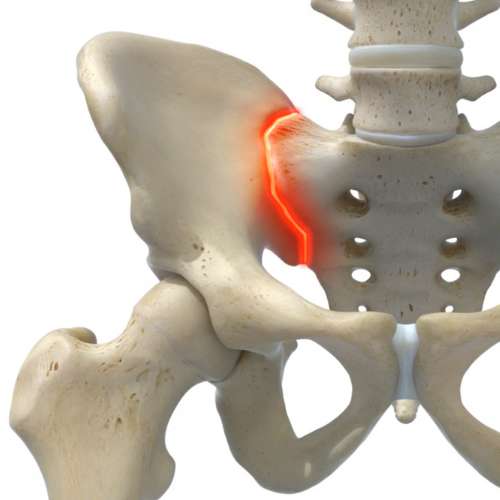
The sacroiliac joints (SI) are the foundation of the spine, located at the junctions of the sacrum and ilium on each side.
These complex joints, composed of systems of ligaments and multiplanar joint surfaces, transmit the forces exerted through the spine from the upper body to the legs. The SI joint is designed to absorb shock forces and is naturally constrained to only limited movement. Instability in the SI joint is a major pain generator in some patients.
Although there have been many advances in surgical techniques to address instability problems in the lumbar spine, instability in the SI joint has remained relatively unaddressed, with most patients running out of options once conservative treatments have failed to offer continued relief from painful SI symptoms.
The opinions expressed are the professional medical opinions and the clinical observations of licensed and practicing physicians and may not necessarily represent claims made by CornerLoc.
Common Causes
of SI Joint Dysfunction
- Prior Injury or Fall
- Car Accident
- Ligamentous Injury
- Post-partum Pelvic Girdle Pain
- Previous Lumbar Spinal Fusion
- Arthritis
- Osteoarthritis
Common Symptoms
of SI Joint Dysfunction
- Pain in lower back
- Commonly one-sided, but it can be both
- Buttocks/Groin Pain
- Pain Radiates into the Pelvis/Upper Thigh
- Dull, sharp, and can create weakness
- A Feeling of Leg Instability/Gait Issues
- Pain or Instability going from Sitting to Standing
- Stiffness in the Pelvis
- Disturbed Sleeping Patterns Due to Pain
- Pain when Weight-bearing on the Leg of the Affected Side
Diagnosis of SI Joint Dysfunction
Step 1
History and Complaints of Pain
Step 2
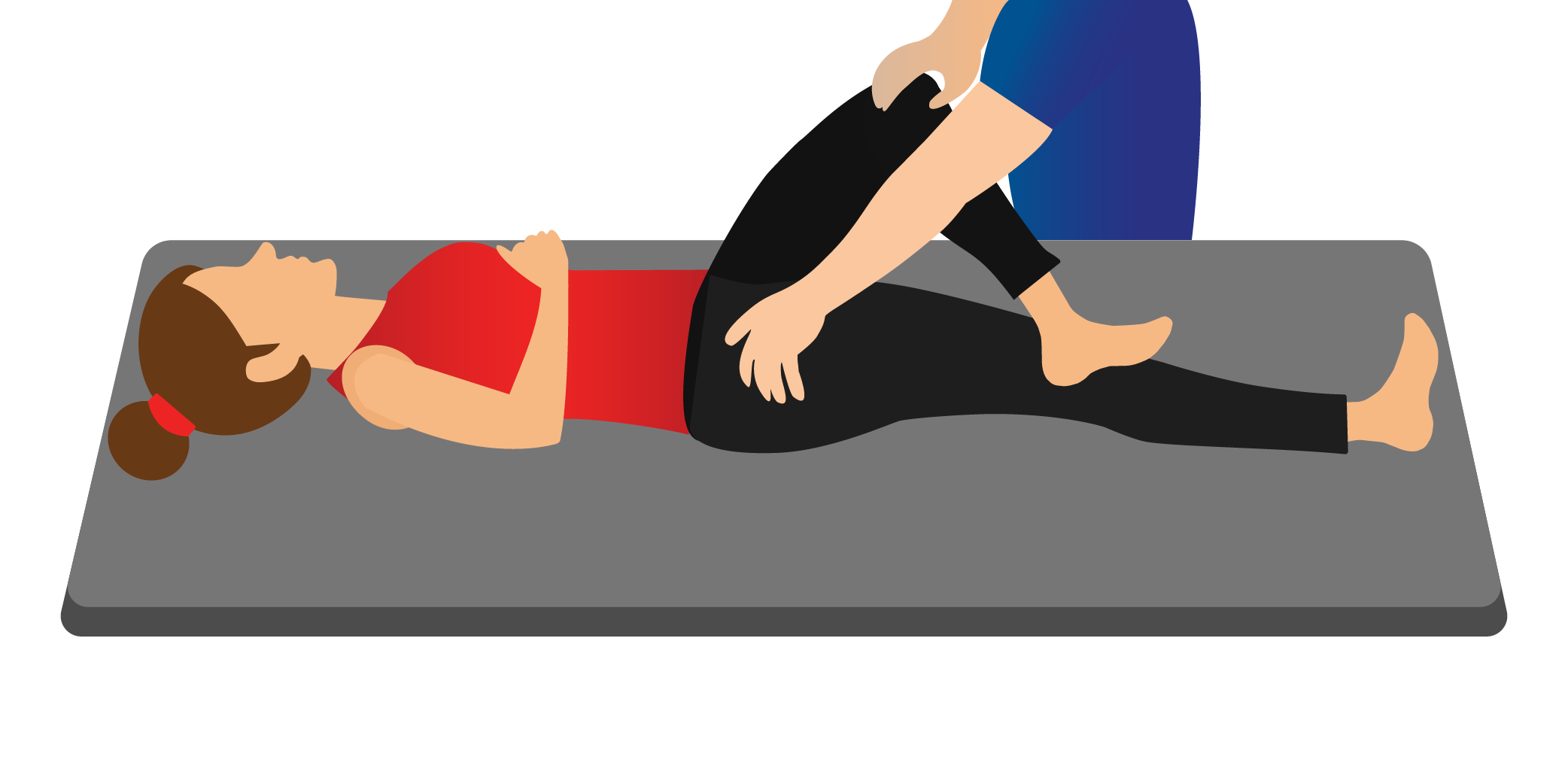
Sacroiliac Joint Examination
- Point to Pain
- Palpate
Step 3
Sacroiliac Joint Dysfunction Five Provocative Tests
The Non-Invasive Process of Identifying Sacroiliac Joint Dysfunction (Mac/LCD guidelines require 3 of 5 positive results)
Step 4
Diagnostic Injections
MAC / LCD Dependent – Typically two injections that give 75% relief
Treatment Cycle and Options
When it is suspected that some or all of a patient’s symptoms could be attributed to SI joint instability, it is recommended to begin with conservative treatment options. Conservative treatment may include physical therapy, chiropractic manipulation, patient specific exercise programs, or bracing.
Pain management evaluation and intervention may be the next step, including pain medications or therapeutic injections that may provide some patients temporary relief, but often only work short term. Radio-frequency ablation (RFA) has also been used with some success, but similar to injections, may only provide temporary relief.
SI joint fusion should only be considered after non-surgical interventions have failed to provide a patient with an enduring solution to their pain. Fusing the SI joint, thereby eliminating pain generating instability, can provide enduring pain relief.

Having Options Matters
Get more information about the SI joint fusion system with options. TransLoc 3D™ and CornerLoc™ GRAFTS allow you the flexibility to create the ideal solution for you and your patients with chronic SI joint dysfunction. Contact us today to have one of our representatives provide you and your practice with more information.